Special Offer: Discounts on Sessions and Memberships!

Medically reviewed by Dr. Lauren Weber, MSCP, ABOM
If you have ever dealt with lingering joint stiffness, stubborn muscle soreness, or that “puffy and achy” feeling that hangs on longer than it should, you have probably run into the topic of inflammation. In the short term, inflammation is part of healing. The problem is when it becomes chronic, staying switched on and quietly contributing to discomfort, slower recovery, and low-grade swelling.
That is where Red Light Therapy and Near-Infrared Photobiomodulation have gained attention. At Deeply Vital Medical, we offer physician-directed, whole-body sessions using Red Light Therapy and Near-Infrared Light in a private studio setting in New York City. The goal is straightforward: support your body’s recovery processes safely and non-invasively, with a plan that fits your needs.
Chronic inflammation is not always loud. It can present as pain, fatigue, headaches, recurring flare-ups, or a sense that your body is slower to bounce back. It is influenced by stress, sleep, dietary intake, activity levels, and underlying health conditions. While you cannot always “feel” inflammation the way you feel a bruise, it often manifests as symptoms people experience day to day.
When people search for treatment for chronic inflammation, they usually hope for options that support comfort and function without adding more complexity to their routine.
In clinical research, Red Light Therapy is a form of Photobiomodulation (PBM). In practical terms, PBM uses specific wavelengths of light that are absorbed by cells and can influence cellular energy production and signaling.
A 2023 literature review by Alberto González-Muñoz and colleagues, published and archived in PubMed Central (PMC), discussed PBM findings across studies of pain and inflammation and described evidence of benefits in certain clinical contexts, while also emphasizing the need for additional high-quality research. That balance matters because it keeps expectations realistic while still acknowledging why PBM remains an active area of study.
When you see the phrase “Photobiomodulation for inflammation,” it refers to the same approach: supporting healthier inflammatory signaling rather than promising a “quick fix.”
Inflammation is often discussed in terms of cytokines, which are chemical messengers that can promote or suppress inflammation.
A 2023 experimental study led by Shamloo and co-authors, published in Frontiers in Neuroscience (a journal from the Frontiers publishing group), examined Photobiomodulation in a mouse model of inflammation. The researchers reported reductions in key pro-inflammatory cytokines (including IL-1β and IL-18) and an increase in an anti-inflammatory cytokine (IL-10). In plain language, the findings suggest that PBM can shift inflammatory signaling in a more favorable direction under certain conditions.
This is a big reason people describe PBM as anti-inflammatory light therapy. It is not positioned as a replacement for medical care, but as a supportive tool that may influence inflammatory biology.
Pain and swelling are commonly tied to inflammatory activity. That is why Red Light Therapy is often discussed alongside recovery, mobility, and comfort.
A 2020 systematic review by R. S. D. Lopes Silva and co-authors, indexed in PubMed, analyzed research on Photobiomodulation in animal models related to tendon injury and tendinitis. The review reported reductions in inflammatory markers and signs of inflammation under specific PBM parameters in the included studies. Animal data is not the same as human clinical evidence, but it is helpful for understanding how PBM may influence tissue-level inflammation and repair pathways.
For someone seeking Red Light Therapy for pain and swelling, the key point is that PBM is being studied not only for symptom relief but also for measurable changes linked to inflammatory signaling.
Inflammation can also involve the nervous system. When the brain and nerves are more inflamed, it can affect how the body experiences pain, stress tolerance, and recovery.A 2022 systematic review led by Fábio dos Santos Cardoso and colleagues, published in Frontiers in Neuroscience and available through PubMed Central, evaluated controlled laboratory animal studies on Photobiomodulation for neuroinflammation. The authors concluded that PBM showed anti-inflammatory effects across multiple neurological models and described transcranial PBM as a promising approach for inflammation-driven neurological conditions, while identifying areas for further research.
That matters because chronic inflammation is rarely “one place only.” It can involve multiple systems, which is part of why whole-body approaches are being explored.
Chronic inflammation can manifest in different forms:
Chronic inflammation acts as a silent catalyst for cancer. It promotes genetic instability and fosters a pro-tumor environment, and this ongoing immune response not only harms cells but also actively supports cancer growth and progression.
Deeply Vital Medical offers relaxing and comfortable physician-directed whole-body sessions using Red and Near-Infrared wavelengths, with Blue Light also available for targeted facial care. Sessions are non-invasive and designed to fit into a wellness routine without downtime.
Here are some reasons patients opt for whole-body light therapy sessions:
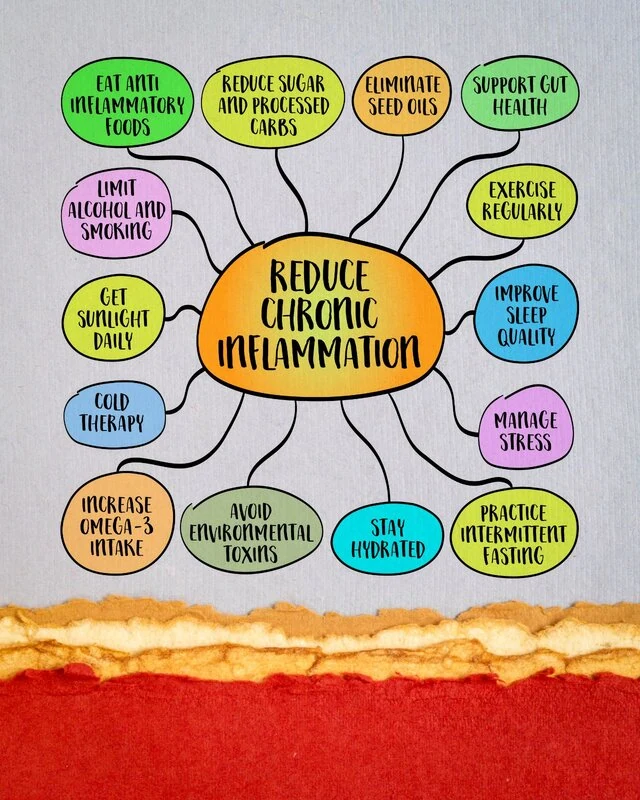
If your goal is to reduce chronic inflammation naturally, consistency matters. Light therapy makes more sense as part of a larger plan, not as a one-time experiment.
People often consider PBM when they are dealing with ongoing discomfort, slow recovery, or a general sense that inflammation is affecting how they feel day to day.
A 2023 research study led by Joo Hee Ryu and colleagues, published in Frontiers in Immunology (Frontiers Publishing Group), explored Photobiomodulation in experimental models of rheumatoid arthritis. The researchers reported improvements in inflammatory parameters in PBM-treated animals, including decreases in pro-inflammatory cytokines and increases in anti-inflammatory cytokines, and discussed inflammatory pathways involved. It is preclinical evidence, but it supports the broader scientific theme that PBM can influence inflammation-related signaling in relevant models.
This is why PBM continues to draw interest as a supportive option alongside lifestyle and medical care.
Chronic inflammation can be frustrating because it rarely has one simple cause. Still, the growing research base around Photobiomodulation suggests it may help influence inflammatory signaling and support recovery, especially when used consistently and thoughtfully. If you are exploring Red Light Therapy in New York, NY, Deeply Vital Medical can help you figure out whether whole-body sessions fit your goals and comfort level.
Learn More About Red Light Therapy and reach out to Dr. Lauren Weber to talk through your concerns, your health history, and what a realistic plan might look like for you.